Abstract
Background. Cardiovascular (CV) events are leading cause of morbidity and mortality in PV. Current risk stratification is based on variables predicting thrombotic risk, ie age >60y and history of thrombosis. Recent studies focused on additional thrombotic risk factors in PV, including generic CV factors and leukocytosis. PV patients (pts) are JAK2V617F mutated, and present wide heterogeneity in variant allele frequency (VAF); it was shown that a VAF >75% was associated with higher number of thrombotic events after diagnosis (Vannucchi AM, Leukemia 2007), but the prognostic role of JAK2 VAF is still debated.
Aim. The aim of the study was to evaluate the impact of JAK2V617F VAF on rate of thrombosis in WHO-2016 defined PV pts.
Patients and Method. In the CRIMM (Florence) database, a total of 577 pts with a JAK2VF VAF determined within 3 years from diagnosis, who met the 2016 WHO criteria for PV, were identified. All pts had information regarding thromboembolic events, including history of thrombosis, occurrence, type and date of thrombosis in the follow-up (FU) and presence of CV risk factors (smoking, hypertension, and diabetes mellitus). Thrombosis‐free survival (TFS) was determined from the time of diagnosis to the time the first thrombotic event occurred. Pts in whom thrombosis did not occur were censored at the time of last FU. Pre-receiver operating characteristic (ROC) plots were used to determine cutoff levels for continuous variables of interest. Differences in the distribution of continuous variables between categories were analyzed by Mann-Whitney or Kruskal-Wallis test. Pts' groups with nominal variables were compared by χ2 test. TFS was estimated by Kaplan Meier analysis; log rank test was used to compare TFS difference between groups. Cox proportional hazards regression was used for multivariable analysis. A two tailed P ≤ 0.05 was considered statistically significant.
Results. The median age of pts at diagnosis was 61y, 308 (53.4%) were above 60y; 57.2% were males. All pts were mutated for JAK2V617F with a median VAF 43% (range 1-100%), 62% had at least one CV risk factor; 83 (14.4%) pts suffered from an episode of thrombosis within 3 yr from, or coincident with, diagnosis. The median FU was 7.3y (0.6-35.9y) during which 87 pts (15.1%) developed thrombosis. (50 arterial and 45 venous thrombosis). During the FU, 110 pts (19.1%) died.
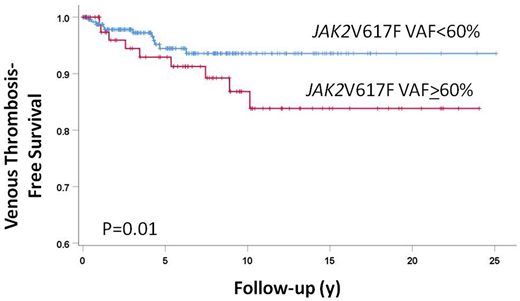
A JAK2VAF of ≥60% cutoff level, as determined by ROC analysis, correlated with measurements of stimulated erythropoiesis (higher hematocrit, lower mean cell volume and serum ferritin; all P<.01), leukocytosis (P<.0001), lower platelets count (P=.02) and elevated serum lactate dehydrogenase (LDH) (P<.03). Pts with ≥60% JAK2V617F VAF were at higher relative risk (RR) of having splenomegaly (RR 3.1; P<0.001), suffering from pruritus (RR 2.5; P<0.001) or constitutional symptoms (RR 1.9; P=0.01), harboring a BM fibrosis grade-1 (RR 3.1; P<0.001). Additionally, pts with a VAF>60% had greater risk to progress to PPV-MF (RR 8.5, P<.0001) and acute leukemia (RR 4.4, P=0.04) or to die (RR 3.8, P<0.0001). The JAK2VF VAF (continuous or ≥60%) did not correlate with occurrence of thrombosis at diagnosis, while the rate of thrombosis during FU was significantly increased in pts with VAF ≥60% (23.4% vs 11.0%, RR 2.4, 95%CI = 1.4-4.0; P<0.0001), more marked for venous (RR 3.7, 95%CI = 2.0-6.8; P<0.0001) than arterial (RR 1.8, 95%CI = 0.9-3.3; P=0.05) thrombosis. The impact of VAF on thrombosis during FU was then estimated according to the conventional risk category. In low risk pts (LR) (n=236), factors significantly associated with occurrence of FU thrombosis were CV risk factors (dyslipidemia (RR 3.3, P = 0.02) and hypertension (RR 1.8, P=0.048)), a G1 BM fibrosis (RR 5.3, P=0.006), presence of splenomegaly (RR, 3.2, P=0.001) or constitutional symptoms (RR 3.3, P=0.003) and a VAF ≥60% (RR 2.2, P = 0.024). In high risk pts (HR) (n=341), factors significant for FU thrombosis were splenomegaly (RR 2.0, P=0.03), elevated LDH (RR 4.0, P=0.009) and a VAF ≥60% (RR 2.3, P = 0.012). A VAF ≥60% was correlated with shortened venous TFS after diagnosis in HR (P = 0.01, HR = 3.2, 95%CI = 1.2−8.3; fig.) but not in LR pts (P = 0.20, HR = 1.1, 95%CI = 0.5−2.9).
Conclusions. This study indicates that conventionally-defined high-risk PV pts with a JAK2V617F VAF ≥60% suffer from increased rate of venous events and might be worthwhile of more intensive antithrombotic prophylaxis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal